In the basement of Surrey Memorial Hospital, in Simon Fraser University’s ImageTech Lab, behind a heavy door plated with copper, lies the MEG.
The magnetoencephalography machine may look like a chic, space-worthy escape pod from Star Trek, but what it does is much cooler — literally and figuratively.
Hidden behind its smooth exterior are 306 sensors resting in a pool of liquid helium, one of the coldest materials on Earth. These sensors let the MEG read minds.
Well, not quite read minds, said Maggie Clarke, associate director and head of the MEG program and adjunct professor at the school of mechatronics systems engineering at SFU.
The MEG can’t tell what a person is thinking, but it reads electromagnetic fields to show researchers what area of the brain is activating, she said.
The goal is to help improve the lives of patients suffering from drug-resistant epilepsy.

Clarke is working to show the Health Ministry why it should invest in its own MEG, which can cost around $3 million.
She’s doing that by running a clinical trial that adds a MEG scan into the lineup of medical tests epileptic patients get before determining if they’re eligible for surgery.
Patients are referred to the trial by their neurologist. They get a scan, that data is given to their health-care team, and then Clarke’s team follows how the patient does after their surgery.
MEGs are a cost-effective way to help reduce how long patients have to stay in hospital and how many brain surgeries they need to treat their epilepsy, Clarke said.
Epilepsy, which results in recurring seizures, can be caused by hundreds of different conditions and is one of the most prevalent neurological disorders, affecting around 50,000 British Columbians or one per cent of the general population, said Mary Connolly, director of BC Children’s Hospital’s comprehensive pediatric epilepsy surgery program and clinical professor in the division of neurology, department of pediatrics, at the faculty of medicine at the University of British Columbia.
Seizures happen when a bunch of neurons fire uncontrollably. Because the brain controls so much of the body, this electrical storm can cause people to lose consciousness, stare off into space or have uncontrolled movements.
Seizures can make regular activities like walking, swimming, driving and playing sports dangerous, Clarke said.
The first line of treatment for epilepsy is medication, but around one-third of cases are drug resistant, Connolly said. Epilepsy can also be treated with dietary therapy, neuromodulation (which acts like a pacemaker for the brain) or surgery.
Surgery can be used to cure most drug-resistant epileptic patients by removing the part of the brain that fires uncontrollably and causes the seizure, Connolly said.
Surgeons will always try to remove as little as they can, she said. In certain rare cases, surgeons can remove half of a child’s brain and have them make a full recovery and go on to live a normal life, seizure-free.
Most children make a “remarkable” recovery after surgery, being discharged from hospital after a week and getting back to school within a month, Connolly said.
The trick is figuring out which exact part of the brain seizures are originating from and calculating the risks of removal. That’s where the MEG comes in.
Brains can adapt and reorganize
Before a surgeon can remove part of a brain, they first need to know what that part of the brain does. Not all brains are organized the same way.
When a young brain is damaged, for example after a stroke, it may be able to reorganize itself to adapt, Connolly said. In certain cases this can include moving the language centre, traditionally in the left side of the brain, to the right side.
The MEG helps doctors map out a patient’s brain to figure out where things like the language and hand movement centres are, as well as what area of the brain the seizures are coming from.
It can do this by sensing “interictal spikes” — signals given off by the part of the brain where the seizures start.
One of the benefits of the MEG is that patients don’t need to have a seizure for the machine to take a reading. The best readings actually happen when patients are sleeping, Clarke said.
SQUIDs and liquid helium
The MEG has 306 sensors hiding inside the smooth plastic indent where a patient rests their head. The sensors are called superconducting quantum interference devices, or SQUIDs, which need to be kept extremely cold to take delicate measurements.
SQUIDs can detect “very, very tiny magnetic fields,” Clarke said.
“When your brain cells communicate it creates [an electrical] current, and when there’s current there’s magnetic fields,” she said. “When large populations of neurons fire and communicate together it creates a current large enough to create a magnetic field outside the head that we can pick up.”
That’s why the MEG is housed in a special room plated with copper and other metals: it needs to rest in a box that blocks out the noisy world of magnetic fields we live in. Electrical current from wires in the hospital, cellphones and even cars driving past would overwhelm the sensors and drown out signals from the brain, Clarke said.
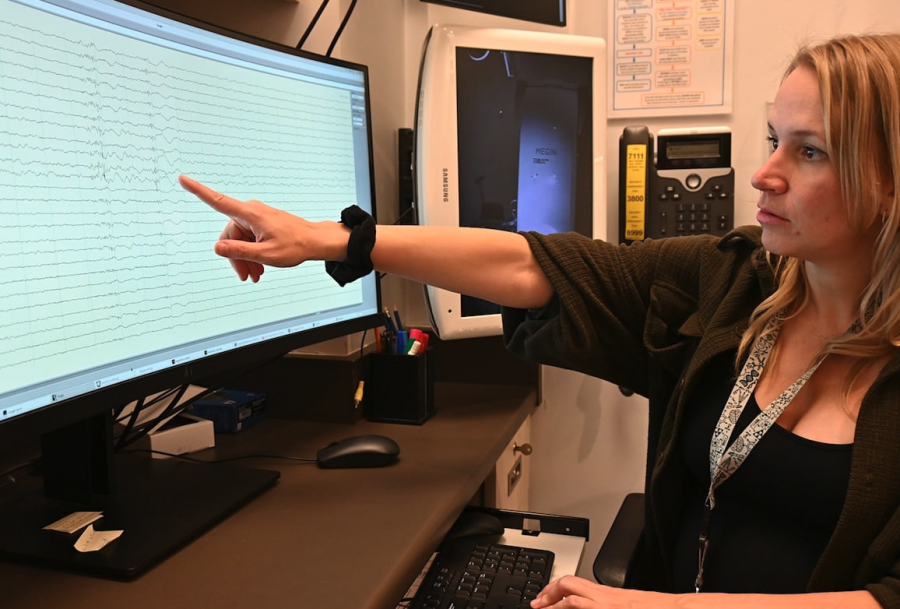
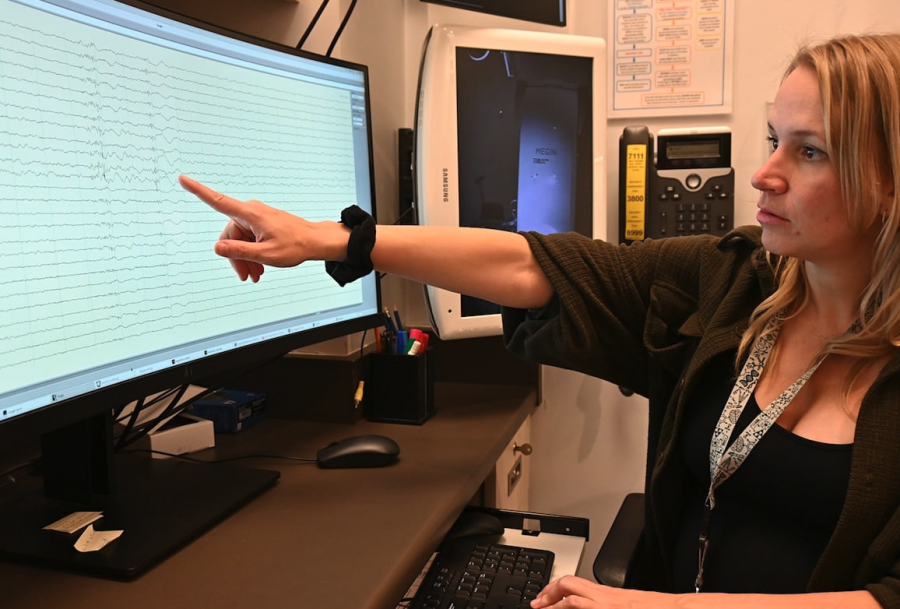
Clarke pointed to a screen showing a MEG reading. Each sensor’s reading was represented by a line wobbling across the display. Occasionally all the lines showed a blip at the same moment, as if someone had run their finger down the screen and smudged them.
That’s what an interictal spike looks like, Clarke said. It allows researchers to pinpoint the general area where the seizures are coming from.
Complementary tests
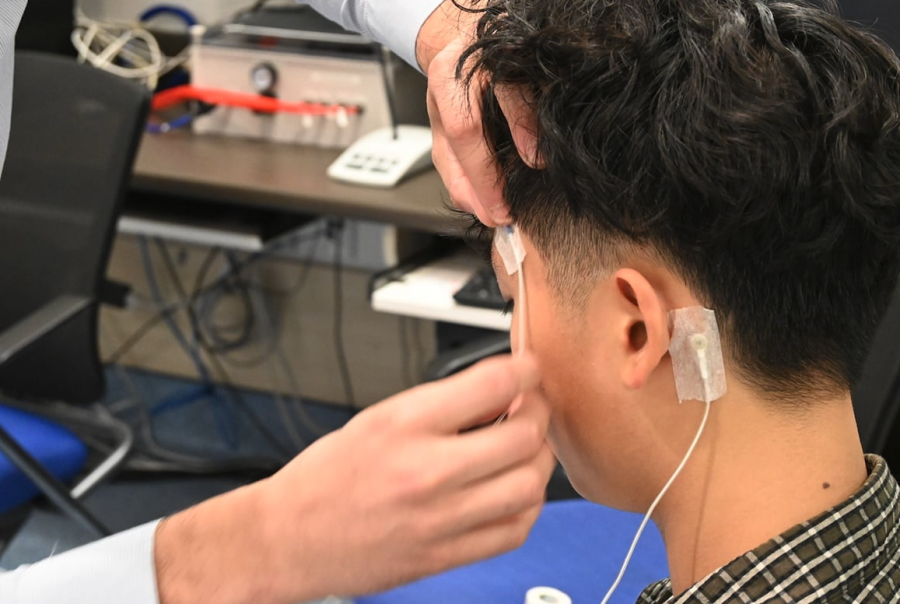
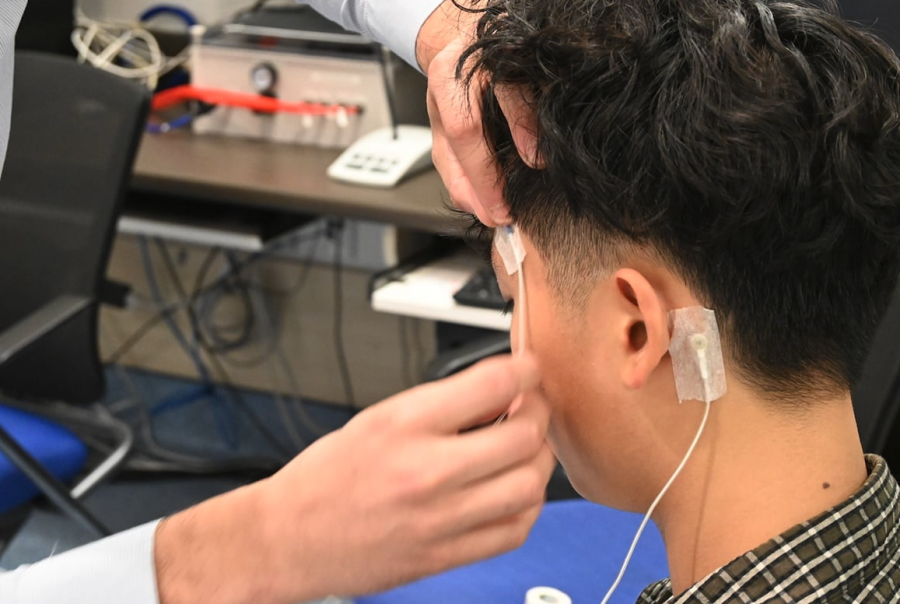
The MEG isn’t the only test that can do this. An electroencephalogram, or EEG, monitoring test can achieve similar results. For that test, however, a patient needs to have a seizure while hooked up to electrodes in a hospital.
That hospital stay is time- and resource-intensive, especially when compared with the MEG, which just requires patients to come in and have a nap, Clarke said.
The MEG also does a better job of zeroing in on where in the brain the seizures are coming from than an EEG, she added, because magnetic fields are not affected by tissue, while the electrical currents picked up by an EEG can be slightly distorted when they travel through the brain and the skull.
After a MEG or EEG monitoring test, patients get a stereo EEG test. This test, which requires surgery to place electrodes on the surface of the brain, further homes in on where the seizures are coming from, Clarke said. However, it’s an incredibly invasive procedure and electrodes can be put on only one small part of the brain at a time.
“If we don’t place them properly we may have to place them again, and that means another surgery,” she added.
The MEG is complementary, rather than replacing other important tests, Clarke said.
It could help cut down on hospital stays if it is used alongside an EEG monitoring test, and the MEG could be used to help identify where to put the stereo EEG electrodes, ideally reducing the odds of the patient having to come back and have another surgery to adjust the electrodes, Clarke said.
The MEG might also show surgeons something other tests miss, she said.
Before a patient is approved for surgery, they will get an EEG, an MRI, a functional MRI and a PET scan, Connolly said, which are all reviewed by their medical team to decide if they could benefit from surgery.
“It’s very individualized,” Connolly said. “Our overall objective is to use the smallest amount of surgery for the maximum benefit.”
“The MEG may allow us to identify more candidates who could benefit from [surgery].”
The clinical trial is in collaboration with BC Children’s Hospital, Fraser Health Authority, Vancouver General Hospital and the University of Alabama at Birmingham.
MEGs are already used clinically in Toronto, the United States and Europe.